How biomedical waste differs from regular waste

Biomedical waste, also known as medical waste or hospital waste, is any kind of waste containing infectious materials generated during the treatment of humans or animals, as well as during research involving biologics. Biomedical, hospital or clinical waste poses a significant risk to human health and the environment if not handled and disposed of properly.
During pre-hospitals the mismanagement of biomedical waste led to severe health crises. The absence of a systematic approach to medical waste handling resulted in appalling practices that contributed significantly to the spread of diseases. Contaminated dressings, surgical instruments, and even human remains were often discarded carelessly in open pits or burned without proper precautions. The lack of basic sanitation measures allowed for the contamination of water supplies and the environment. To conserve resources, medical equipment was frequently reused without adequate sterilization, exacerbating the risk of infection transmission.

Taught by these mistakes, we shouldn’t take medical waste management lightly and try to educate in this field more. Let’s get it started.
Categories of Biomedical Waste
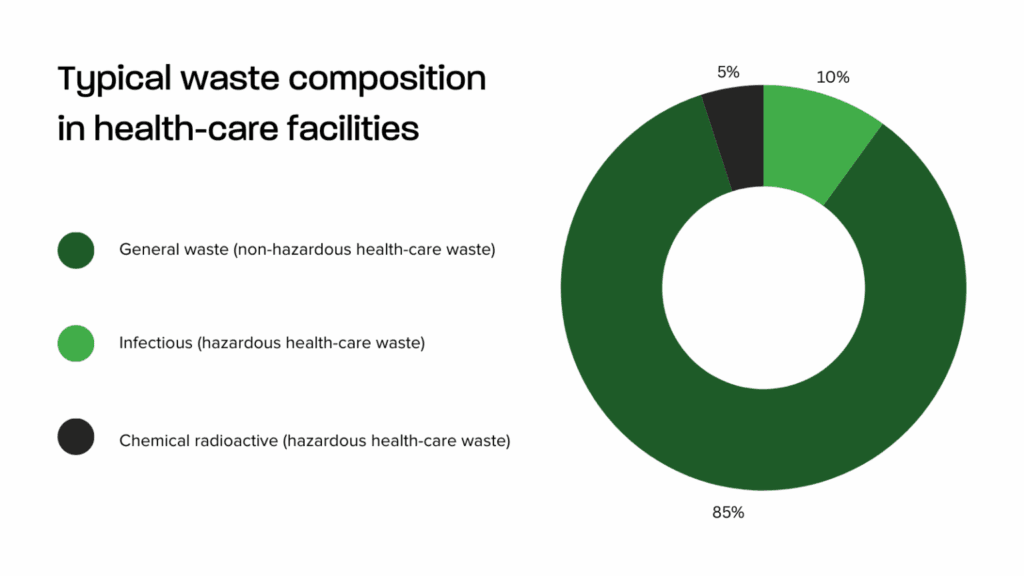
For understanding the differences between biomedical waste let’s look at 8 main types based on WHO:
- Infectious waste: waste from laboratory operations, including infectious agent cultures and stocks as well as wasted diagnostic samples contaminated with blood and other body fluids. trash from autopsies, contaminated laboratory animals, and sick patients’ bodies (swabs, bandages, and disposable medical equipment);
- Pathological waste: human body parts, tissues,& fluids, and contaminated animal carcasses;
- Sharps waste: syringes, needles, disposable scalpels and blades, etc.;
- Chemical waste: all solvents and reagents used for laboratory preparations, testing, disinfectants, sterilant and heavy metals contained in medical device.
- Pharmaceutical waste: pharmaceutical drugs, immunization vaccine etc.
- Cytotoxic waste: waste containing substances with genotoxic properties such as cytotoxic drugs used in cancer treatment and their metabolites;
- Radioactive waste: such as products contaminated by radionuclides including radioactive diagnostic material or radiotherapeutic materials.
- Non-hazardous or general waste: waste that does not pose any particular biological, chemical, radioactive or physical hazard.
Waste management
Now, how is biomedical waste management different from regular waste management? Let’s compare them starting with regular waste management:

Regular waste management:
1. Generation:
- Waste is produced from various sources, including households, industries, and commercial establishments.
2. Collection:
- Waste is gathered from different locations and transported to designated collection points.
3. Transportation:
- Collected waste is transported to processing or disposal facilities.
4. Treatment:
- Waste undergoes various treatments depending on its type:
- Recycling: Converting waste into new materials.
- Composting: Organic waste is broken down into nutrient-rich compost.
- Incineration: Burning waste to reduce volume and generate energy.
- Landfilling: Disposing of waste in a controlled landfill.
5. Disposal:
- Treated or untreated waste is ultimately disposed of in landfills or other designated areas.
Biomedical waste management can be summarized in the following steps:
1. Waste segregation is carried out in color-coded and barcode-labeled bags/containers at the source of generation:
Waste segregation practices should be standardized nationwide, guided by national healthcare waste management guidelines and legislation. A uniform color-coding system should be implemented to visually indicate the potential risk posed by the waste in each container, making it easier to correctly dispose of waste and maintain segregation during transport, storage, treatment, and disposal.
Segregation of waste should be done by using containers of different colors. Labeling waste containers is essential for identifying the source, recording the type and quantities of waste produced in each area, and tracing any segregation issues back to their point of origin. Using an international hazard symbol on each waste bag is recommended if not already applied.
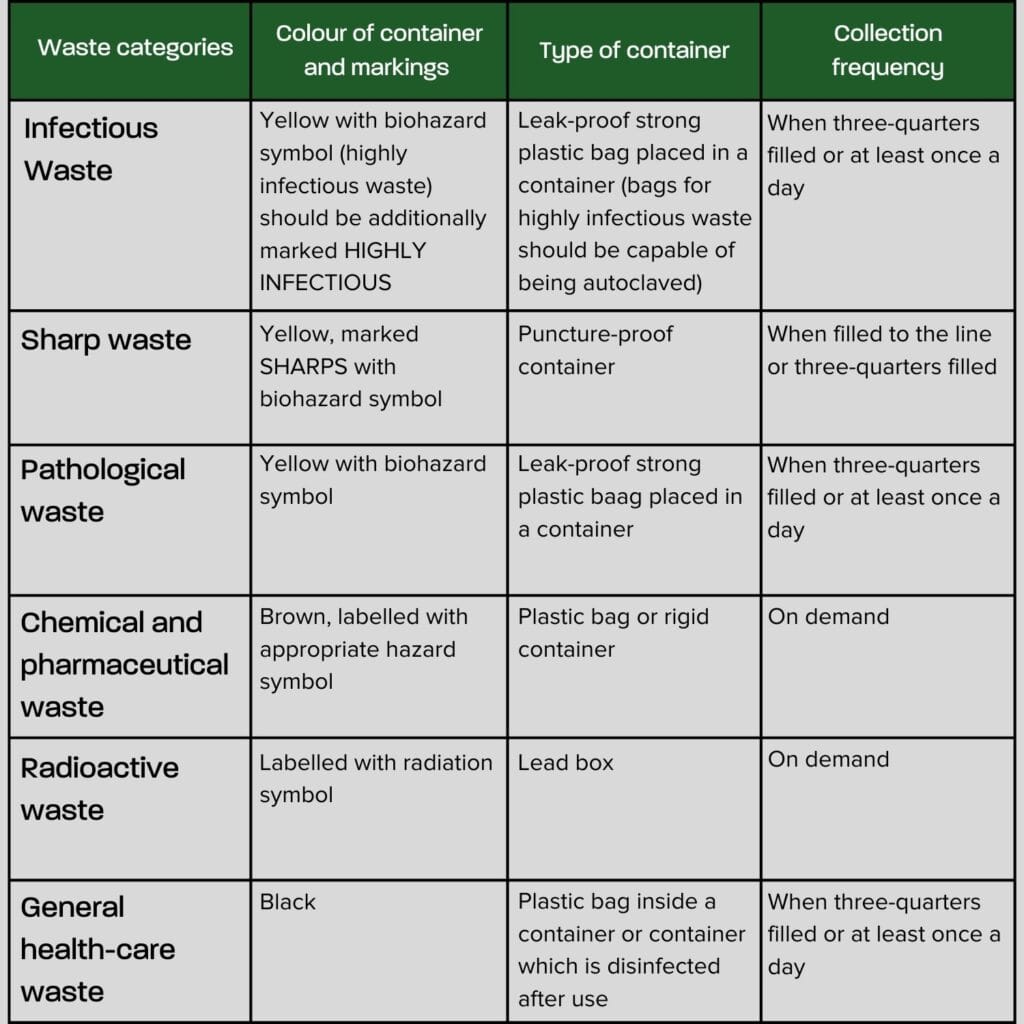

Containers for infectious waste should not be placed in public areas to prevent patients and visitors from coming into contact with potentially infectious materials. Instead, infectious waste bins should be located as close as possible to where waste is generated, such as nursing stations, procedure rooms, or points of care.

2. Pre-treat Laboratory and Highly infectious waste:
Pre-treatment is essential for reducing the volume, weight, and pathogenicity of biomedical waste. The choice of pre-treatment method depends on the waste type, volume, and potential hazards. Common methods include disinfection, autoclaving, incineration, and chemical treatment. Disinfection is used to kill microorganisms on surfaces and equipment. Autoclaving, involving high temperature and pressure, is effective for sterilizing infectious and pathological waste. Incineration, while reducing waste volume, should be considered carefully due to environmental concerns. Chemical treatment is employed to neutralize or inactivate hazardous components.
3. Intra-mural transportation of segregated waste to central storage area
Intra-mural transportation is a critical step in biomedical waste management. It involves the careful movement of segregated waste from its origin within a healthcare facility to a central storage area. To ensure safety and prevent contamination, dedicated transportation routes should be established. Waste must be contained in leak-proof and sturdy containers. Staff responsible for transportation should be well-trained in handling biomedical waste and equipped with appropriate personal protective equipment. Additionally, comprehensive spill response plans are essential to address any accidents that may occur during transport.

4. Temporary storage of biomedical waste in central storage area:
The central storage area serves as a temporary holding place for biomedical waste before treatment or disposal. It is crucial to select a secure and isolated location, away from patient care areas, for the storage area. Proper storage conditions, including temperature, humidity, and lighting, must be maintained. Containers should be intact and securely sealed. Access to the storage area should be restricted to authorized personnel only. Regular inspections are necessary to identify any potential issues such as leaks, damages, or pest infestations.
5. Treatment and Disposal of biomedical waste through CBWTF or Captive facility
The final stage involves the treatment and disposal of biomedical waste. Treatment methods, such as incineration, autoclaving, microwave disinfection, or chemical treatment, are selected based on waste type and volume. The waste is processed in either a common biomedical waste treatment facility (CBWTF) or a captive facility on-site. Adherence to local, state, and federal regulations is paramount throughout the process. Detailed records of treatment and disposal activities must be maintained. Additionally, a thorough environmental impact assessment should be conducted to evaluate the potential consequences of the treatment process.

Understanding the stark differences between biomedical waste management and regular waste disposal is crucial for protecting public health and the environment. Unlike everyday garbage, biomedical waste often contains infectious agents, hazardous chemicals, and sharp objects that pose significant risks. And perhaps the same question has occurred to all of us: What would happen if biomedical waste was handled like regular waste? I suppose the consequences could be really bad :
- Spread of diseases: Improper disposal can contaminate water supplies, soil, and air, leading to outbreaks of infectious diseases.
- Injury: Sanitation workers and the public could be exposed to sharp objects, resulting in serious injuries.
- Environmental damage: Toxic chemicals and hazardous substances can harm wildlife and pollute ecosystems.
- Public health risk: Biomedical waste can attract pests like rats and insects, which can spread diseases.

Here’s a prime example of a hospital implementing innovative biomedical waste management practices: Cleveland Clinic in the United States. Cleveland Clinic is dedicated to minimizing waste and diverting materials from landfills through the following waste management strategies:
- Comprehensive Waste Systems
Cleveland Clinic manages 37 distinct waste streams across its facilities, ranging from general waste like paper and food to specialized and hazardous materials like lab chemicals and biohazards. Each waste stream is managed with tailored processes, compliance protocols, and educational programs to ensure safe disposal, effective landfill diversion, and cost efficiency. - Source Reduction
The Clinic focuses on preventing waste at its source through environmentally conscious purchasing. This includes encouraging vendors to reduce packaging, use reusable pallets, and offer recyclable or biodegradable options. Strategies like just-in-time inventory, optimizing supply storage, and ensuring kits contain only necessary items help cut down on unnecessary waste. Additionally, the use of IoT-enabled devices for patient monitoring reduces environmental impact by optimizing care delivery. - Recycling and Reprocessing
Their recycling programs are comprehensive, covering everything from common recyclables like paper and metal to specialized streams like single-use medical devices. By reprocessing these devices, Cleveland Clinic not only reduces waste but also reintegrates sanitized instruments back into operations. - Turning Waste into Value
Cleveland Clinic constantly seeks creative ways to repurpose materials. One standout example is their initiative to recycle operating room packaging. When no existing market was available for this material, they established a new one, connecting their waste hauler to it and designing a safe collection process. This program has since been shared with hospitals nationwide. - Hazardous and Regulated Medical Waste
Cleveland Clinic handles hazardous and regulated medical waste with the highest safety standards. Strict policies guide the safe handling, storage, and transportation of these materials. In 2022, the Clinic managed 76 tons of hazardous waste domestically, ensuring that only truly hazardous materials are processed accordingly. They do not ship hazardous waste internationally, focusing solely on safe domestic management.

If you’re inspired by the practices at Cleveland Clinic, you can take the next step in modernizing your waste management with Sensoneo’s smart solutions. Our advanced products bring the same level of innovation to your facility, helping you achieve efficiency, safety, and sustainability in managing medical waste.
Our robust system, powered by smart ultrasound and radar sensors, can be installed directly in specialized medical waste containers. These sensors continuously monitor fill levels, providing real-time data to our waste management platform. With this information, you can optimize your hazardous waste pickups—saving time, resources, and ensuring regulatory compliance. Streamline your operations while prioritizing safety with Sensoneo’s intelligent medical waste management system.

Sources: beckershospitalreview.com, my.clevelandclinic.org, cureus.com, iris.who.int, psidispo.com
Latest waste library articles

How might the Deposit Return Schemes look like in future?
Deposit Return System
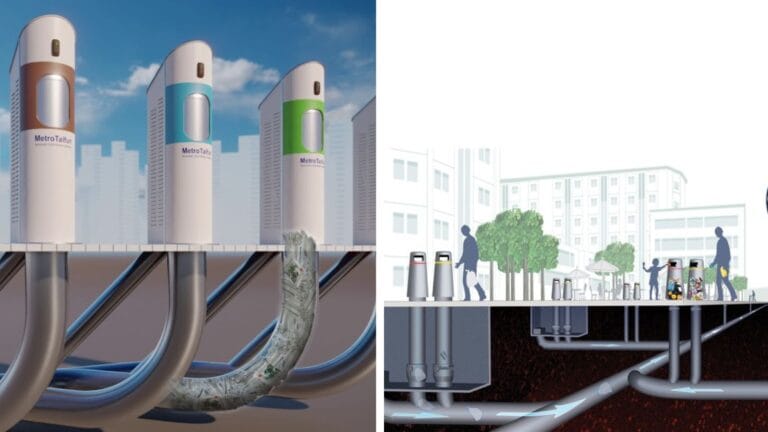
The 3 essentials of an automated vacuum waste collection system
Waste Collection
Top 20 Manufacturing companies ranked by ESG waste score
Factory Waste Management, Waste Collection
ESG Reporting made clear: Compliance & best practices
Factory Waste Management
Smart Waste Newsletter
Get monthly updates from our company and the world of waste!